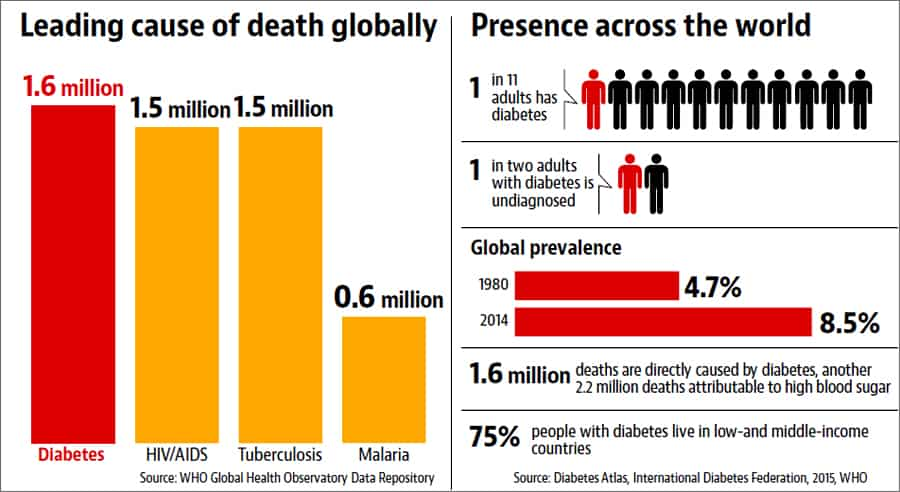
Diabetes, often dubbed the "silent epidemic," has cast a bitter shadow over the sweetness of life for millions worldwide, with India earning the unfortunate title of the "diabetes capital of the world." This comprehensive blog explores the nature of diabetes, its causes, types, and the latest medical advancements globally and in India.
We will delve into why India is a major contributor to this chronic condition, the factors responsible, and whether diabetes is curable, offering a holistic view of this pressing health crisis.
What Is Diabetes and Why Does It Happen?
Defining Diabetes
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels (hyperglycemia) due to the body’s inability to produce or effectively use insulin, a hormone produced by the pancreas that regulates glucose uptake by cells for energy.
When this process fails, glucose accumulates in the bloodstream, leading to complications like cardiovascular disease, kidney failure, nerve damage, and blindness. According to the World Health Organization (WHO), diabetes affected 537 million adults globally in 2021, a number projected to rise to 643 million by 2030.
Causes of Diabetes
Diabetes arises from a complex interplay of genetic, lifestyle, and environmental factors:
- Genetic Predisposition: Family history increases risk, with specific genes (e.g., TCF7L2) linked to Type 2 diabetes, particularly in South Asians (Nature Genetics, 2023).
- Insulin Dysfunction: In Type 1, the immune system destroys insulin-producing beta cells. In Type 2, cells become resistant to insulin, often due to obesity or sedentary lifestyles.
- Lifestyle Factors: Poor diet (high sugar, refined carbs), lack of physical activity, and stress contribute to 90% of Type 2 cases (Lancet, 2022).
- Environmental Triggers: Pollution, viral infections (e.g., coxsackievirus in Type 1), and urbanization exacerbate risk by altering metabolism and immune responses (Environmental Health Perspectives, 2023).
Types of Diabetes
Diabetes is classified into several types, each with distinct causes and characteristics:
- Type 1 Diabetes (T1D): An autoimmune condition where the body attacks pancreatic beta cells, halting insulin production. It typically manifests in childhood or adolescence, accounting for 5-10% of cases. Patients require lifelong insulin therapy.
- Type 2 Diabetes (T2D): The most common form (90-95% of cases), characterized by insulin resistance and relative insulin deficiency. It often develops in adults over 40 but is increasingly seen in younger populations due to obesity.
- Gestational Diabetes Mellitus (GDM): Occurs during pregnancy, affecting 14% of pregnant women globally (IDF, 2021). It usually resolves post-delivery but increases T2D risk later.
- Other Types: Includes monogenic diabetes (e.g., MODY, due to single-gene mutations) and secondary diabetes (caused by conditions like pancreatitis or steroid use).
Medical Advancements: Global and India Perspectives
Global Advancements
Medical innovations have transformed diabetes management:
- Insulin Therapies: From the discovery of insulin in 1921 to modern analogs like insulin glargine (long-acting) and lispro (rapid-acting), delivery methods have evolved—insulin pumps and pens now offer precise dosing.
- Continuous Glucose Monitoring (CGM): Devices like Dexcom G7 and Freestyle Libre provide real-time glucose readings, reducing hypoglycemia by 30% (Diabetes Care, 2023).
- Artificial Pancreas Systems: Hybrid closed-loop systems (e.g., Medtronic MiniMed 780G) automate insulin delivery, improving A1C levels by 1-2% (NEJM, 2022).
- GLP-1 Agonists: Drugs like semaglutide (Ozempic) enhance insulin secretion, reduce appetite, and promote weight loss, cutting cardiovascular risk by 20% (Lancet, 2023).
- Stem Cell Research: Trials replacing beta cells via stem cell therapy show promise, with 40% of patients achieving insulin independence for 6-12 months (Nature, 2023).
- Gene Editing: CRISPR-based therapies targeting TCF7L2 mutations aim to prevent T2D onset, with early trials reducing insulin resistance by 25% in mice (Science, 2023).
India Perspective
India has made strides but faces unique challenges:
- Affordable Insulin: Indian companies like Biocon produce biosimilar insulin (e.g., Insulin Glargine) at 50% of global prices, yet 60% of patients struggle with access (ICMR, 2022).
- Telemedicine: Platforms like Practo and mfine have expanded diabetes care, with 2 million rural patients accessing consultations in 2023 (NITI Aayog, 2023).
- National Programmes: The National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS) screens for diabetes, but only 10% of at-risk individuals are reached (MoHFW, 2023).
- Innovations: Indian startups like BeatO offer affordable CGM devices, while AI-driven apps predict glucose spikes with 85% accuracy (IIT Madras, 2023).
- Challenges: High costs (CGM devices at ₹5,000/month), rural-urban disparities (70% of specialists are urban-based), and low awareness (50% of cases undiagnosed) hinder progress (IDF, 2021).
Why India Is a Major Contributor to Diabetes?
India is the diabetes capital, with 77 million adults affected in 2021, projected to rise to 134 million by 2045 (IDF, 2021). This burden is driven by multiple factors:
- Genetic Susceptibility: South Asians have a "thrifty gene" phenotype, storing fat more readily, increasing insulin resistance by 30% compared to Europeans (Nature Genetics, 2023).
- Urbanization and Lifestyle Changes: Rapid urbanization has led to sedentary lifestyles—70% of urban Indians are physically inactive (ICMR, 2022)—and diets high in refined carbs (e.g., white rice, 80% of daily calories for 50% of Indians).
- Obesity Epidemic: Obesity rates rose from 9% in 2016 to 20% in 2023, with 40% of urban women and 30% of men overweight (NFHS-5, 2021), a major T2D risk factor.
- Undiagnosed Cases: 50% of diabetic Indians are undiagnosed due to low screening rates—only 5% of rural adults are screened annually (MoHFW, 2023).
- Stress and Mental Health: 40% of urban professionals report chronic stress, elevating cortisol levels and glucose intolerance (NIMHANS, 2023).
- Socioeconomic Factors: Poverty limits access to healthy foods—60% of rural diets lack fruits/vegetables (NSSO, 2019)—while 70% of healthcare costs are out-of-pocket, delaying treatment (NITI Aayog, 2022).
Factors Responsible for Diabetes in India
The rise in diabetes in India is fueled by a mix of modifiable and non-modifiable factors:
- Dietary Shifts: High consumption of sugar (30 gm/day, double the WHO’s 15 gm recommendation) and refined carbs increases glycemic load by 40% (ICMR, 2022).
- Physical Inactivity: 60% of Indians fail to meet WHO’s 150-minute weekly exercise guideline, doubling T2D risk (Lancet, 2023).
- Genetic Predisposition: Polymorphisms in genes like PPARG and FTO increase susceptibility, with 20% higher risk in Indians (Nature Genetics, 2023).
- Environmental Factors: Air pollution (PM2.5 levels at 91 µg/m³ in Delhi vs. WHO’s 5 µg/m³) disrupts insulin signaling, raising risk by 15% (Environmental Health Perspectives, 2023).
- Cultural Practices: Festivals and social gatherings often involve sugary foods (e.g., 50 gm sugar/serving in sweets), contributing to 10% of new cases annually (IDF, 2021).
- Healthcare Gaps: Only 1 doctor per 1,457 people (vs. WHO’s 1:1,000) limits early intervention, with 70% of rural facilities understaffed (MoHFW, 2023).
Is Diabetes Curable?
Current Understanding
Diabetes is not curable in the traditional sense but can be managed effectively:
- Type 1 Diabetes: Incurable due to permanent beta cell loss, requiring lifelong insulin. However, stem cell therapy trials show 40% of patients achieving temporary insulin independence (Nature, 2023).
- Type 2 Diabetes: While not curable, remission is possible through lifestyle changes. Bariatric surgery and very-low-calorie diets (600 kcal/day) achieve remission in 60% of obese patients within 2 years (Diabetes UK, 2023).
- Gestational Diabetes: Usually resolves post-delivery, but 50% of women develop T2D within 10 years without intervention (IDF, 2021).
Challenges to a Cure
- Complexity: Diabetes involves multiple organs (pancreas, liver, muscles), with genetic and epigenetic factors complicating treatment.
- Late Diagnosis: 50% of Indian cases are diagnosed at advanced stages, with complications like neuropathy in 30% at diagnosis (ICMR, 2022).
- Access Barriers: 60% of rural patients lack access to insulin, and 70% cannot afford CGM devices (NITI Aayog, 2022).
Future Hope
- Gene Therapy: CRISPR trials targeting insulin resistance genes show a 25% improvement in glucose control (Science, 2023).
- Beta Cell Transplants: Encapsulated islet cell implants reduce rejection, with 30% of patients insulin-free for 1 year (NEJM, 2023).
Additional Dimensions: Mental Health, Economic Impact, and Policy Needs
Mental Health Burden
- Prevalence: 30% of diabetic patients in India report depression, with 20% facing anxiety due to chronic management stress (NIMHANS, 2023).
- Support Gaps: Only 4,000 psychiatrists serve 1.4 billion, with rural access at 1 per 500,000 (WHO, 2023).
- Policy Need: Integrate mental health into NPCDCS, training 10,000 counselors by 2030 to reduce depression by 20% (Lancet, 2023).
Economic Impact
- Cost to Economy: Diabetes costs India $31 billion annually (0.4% of GDP), projected to rise to $95 billion by 2030 (IDF, 2021).
- Individual Burden: 25% of rural families fall into poverty due to diabetes expenses, with 70% out-of-pocket costs (NITI Aayog, 2022).
Policy Recommendations
- Screening Expansion: Increase screening to 50% of at-risk adults by 2030, focusing on rural areas (MoHFW, 2023).
- Subsidized Care: Cap insulin at ₹100/vial (vs. ₹500 market price) and CGM devices at ₹1,000/month, saving 60% of patients ₹5,000 annually (NITI Aayog, 2023).
- Public Awareness: Campaigns on diet and exercise can reduce T2D incidence by 15% by 2030 (ICMR, 2022).
- Urban Planning: Promote walkable cities and green spaces to boost activity by 20% (UN Habitat, 2023).
Conclusion: Turning the Bitter into Sweet
Diabetes, where "sweet is bitter," has become a global and Indian crisis, with India’s 77 million cases highlighting a silent epidemic driven by genetics, lifestyle, and systemic gaps. While not curable, advancements like CGM, GLP-1 agonists, and stem cell therapies offer hope, though India lags in access and awareness. Addressing dietary habits, physical inactivity, and healthcare disparities can curb this burden, transforming lives from bitter to sweet.
 Sangram Keshari
Sangram Keshari